This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
A 14 yr old male came to the opd with chief complaints of pain abdomen in left upper quadrant since 1month
HOPI: PAatient was apparently asymptomatic performing his daily routine activities until 3 months ago , then he noticed a mass in left upper quadrant which is progressive in nature upto umbilicus which is painless , then on 24/10/22 back,he developed loss of appetite and dull ache pain , which is insidious in onset in left upper quandrant , dragging type of pain continuous , aggravated on deep inspiration and partially relieved by medication associated with 2 episodes of vomiting which is non bilious, the mass now rapidly increased below umbilicus .
h/o cough with sputum since 3 days after bronchoscopy
No history of fever (to rule out leishmania and malaria)
No history of weight loss, night sweats( to rule out malignancy)
no history of constipation and diarrhea.
PAST HISTORY
NO history of blood transfusions
NO history of seizures
On further asking parents ,they told he used to have recurrent colds ,cough and fever .He used inhalers for 1 year during winters in childhood .
FAMILY HISTORY:
He is a 4th order child ,born out of grade 4 consanguinous marriage
His sister , who was the first child expired at 5 years due to complications of spleenomegaly
PERSONAL HISTORY:
Diet : MIxed
sleep : adequate
appetite:normal
bowel and bladder regular
no habits
Daily activities: As he is a hostellite in gurukul, he wakes up at 4 0 clock ,freshen up does running and some exercises which are fatiguable for him than their friends , he takes thyroid tablet and freshen up, he eats breakfast , then he goes to school , he sits in first bench as he has a visual acuity of -4.2 and at 12 0 clock he eats lunch (except brinjal) , unitil 6 0 clock he has classes and then plays and have dinner and goes to sleep at 9pm .He have leg pains at night( restless leg syndrome?)
TREATMENT HISTORY:
he was on thyroxine 50 micrograms
GENERAL EXAMINATION:
On 30/11/22
patient is conscious , coherent and cooperative, thin built
height -156 cm
weight-32 kgs
conjuctival pallor +
icterus -
cyanosis -
clubbing-
lymphadenopathy cervicAl , can be palpated in 1B 0.5×0.5 cm firm non tender skin pinchable over the skin
Axillary , inguinal ( not given consent)
waldeyer ring
tonsils:
edema -
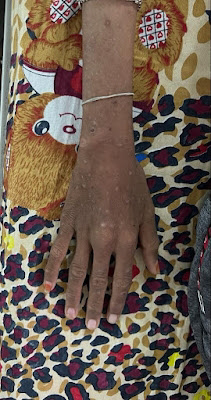
skin - chicken pox scars are seen
healed leg ulcers.
VITALS
BP: 110/70mm Hg in right brachial artery
pulse rate: 82 bpm regular, normal volume, normal character, normal peripheral pulses
temperature: afebrile
respiratory rate: 16cpm
SYSTEMIC EXAMINATION:
Abdomen : Soft , tender
spleenomegaly: firm, non tender , smooth surface 2cm beyond the umbilicus, moving with respiration
no free fluid.
CVS: apex beat in 5th intercoastal space 1cm medial yo mid clavicular line
s1 , s2 heard
RESPIRATORY SYSTEM: normal vesicular breath sounds all areas .no added sounds
CNS:
E4, V5,M6
No focal neurological deficits
on examination -
He was thin built .
Height -156 cm
Weight - 32kgs
Jaundice + ,pallor +
Per abdomen -soft, non tender with moderate splenomegaly
Outside investigations -
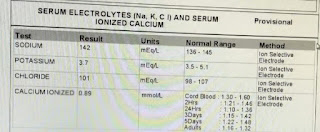
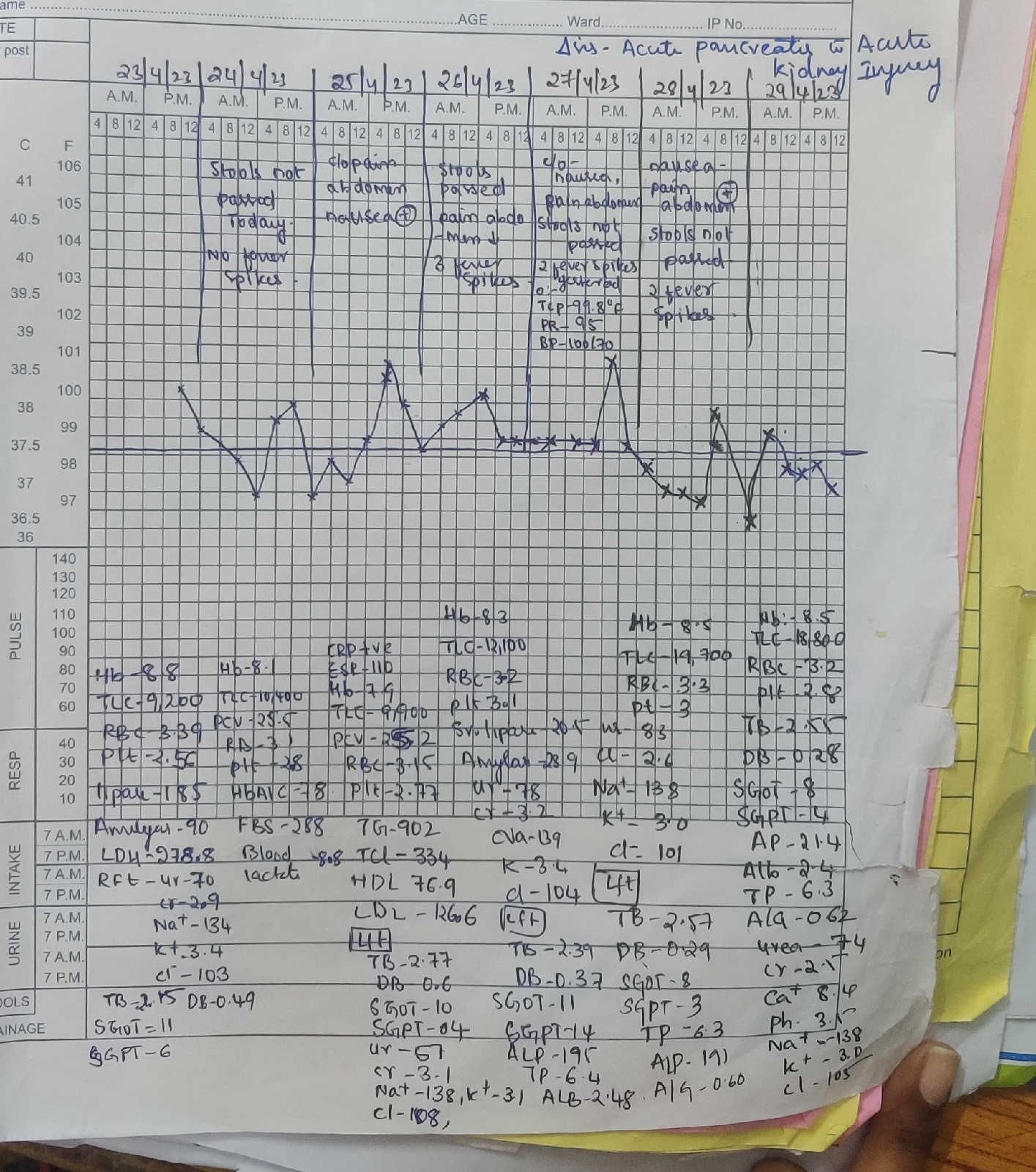
There is significant drop in hemoglobin from 8.9 to recent HB -5,leucopenia , thrombocytopenia.
With raised bilirubin - both direct and indirect, normal enzymes .
Urine for bile salts and bile pigments + ve
HB electrophoresis - normal .
Serology for HiV ,HBSag , Hcv was negative
Dengue , Malaria ,widal was negative
Hemogram showed -
Normocytic normochromic anemia with HB 5.1
WBC count -1700 ,neutrophils -39% ANC-663 ,Esoniphils -8% .
Platelet count -1.5 lakh
With few microcytes ,tear drop cells ,pencil forms.
Liver profile showing total bilirubin of 6.49, direct amounting to 0.52, with AST,ALT,ALP normal, total proteins of 5.5 and albumin of 3.8
Direct Coombs was positive
USG abdomen showing moderate splenomegaly.
Assessment :
? Spectrum of Autoimmune diseases -
Thyroditis ,? AIHA (warm body type) CVID
He was started on methylprednisalone 32mg IV for 5 days later on converted to oral dosage of 30mg and was tapered over 2 months.
And vitamin B12 1000mcg injections through the course of hospital and was continued for 6 months (standard b12 regimen ). And other symptomatic medications.
Provisional diagnosis: spleenomegaly (hyperspleenism) 8cm below left costal margin with anemia and generalized lymphadenopathy
Differential diagnosis
Gaucher disease
Sarcoidosis
Autoimmune haemolytic anemia with thyroiditis,cvid, leukaemia
INVESTIGATION
From 11/11/22
Peripheral smear
With due consent from Dr.Raveen sir ,his management taken
Chest x ray PA view
ECG
He was referred to higher centre in view of portal hypertension secondary to ?NCPH/IPH, given the background of hypersplenism, massive splenomegaly with liver profile normal, portal vein doppler showing portal vein of diameter 1.6cms, with patent hepatic artery and vein, no collaterals and no ascites
He was also treated for tropical spleen with primaquine 30mg for 2 weeks, artemether and lumefantrine.
Bone marrow biopsy and lymph node biopsy showed reactive with no evidence of infiltrative etiology or malignancy in September.
CT SCAN
brochoalvelar lavage was advised to see halo sign to rule out fungal etiology
Brochoscopy video
https://youtu.be/Iq74qwi5Aws
DEFINITIVE DIAGNOSIS
Rosai dorfman syndrome WITH SPLEENOMEGALY
plan of treatment
.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly
Definitive management spleenomegaly
Halo sign differentials?
hemorrhagic nodules of infectious origin (mucormycosis, candidiasis, tuberculosis, viral pneumonia, and invasive aspergillosis--the last being the most common cause of the CT halo sign); hemorrhagic nodules of noninfectious origin (Wegener granulomatosis, Kaposi sarcoma, and hemorrhagic metastases); tumor cell infiltration (bronchioloalveolar carcinoma, lymphoma, and metastasis with intra-alveolar tumor growth); and nonhemorrhagic lesions (sarcoidosis and organizing pneumonia)
Emperipolesis (a megakarocyte containing neutrophils)also seen in myelodysplastic syndrome, myeloproliferative neoplasms, chronic lymphocytic leukemia
Credits and reference :
https://raveen7795.blogspot.com/2022/11/14m-massive-splenomegaly.html

























Comments
Post a Comment